MEG stands for magnetoencephalography, which records magnetic signals that are emitted due to the activity of neurons in the brain. Results are visualised in curves comparable with brain wave curves generated during EEG which shows the brain activity. An epilepsy patient's curve of electric and magnetic signals measurable in the brain has a characteristic pattern.
MEG, like EEG, is a purely diagnostic procedure without radiation exposure or other side effects and is used to determine which brain structures cause, or contribute to causing, the seizures. In special cases, apart from recording spontaneous brain activity, MEG can also ascertain which areas of the brain are directly necessary for processing touch, movements, hearing and sight.
When is MEG used?
MEG is not a routine procedure. Our Epilepsy Centre is the only centre in Germany which has its own system. It is specifically used for patients with focal epilepsy, in whose case seizure freedom cannot be achieved by medication and who might therefore qualify for brain surgery. MEG examinations are not used for patients who are almost entirely free of seizures due to medication. Whether or not magnetoencephalography makes sense is decided on a case-by-case basis depending on various other examination results.
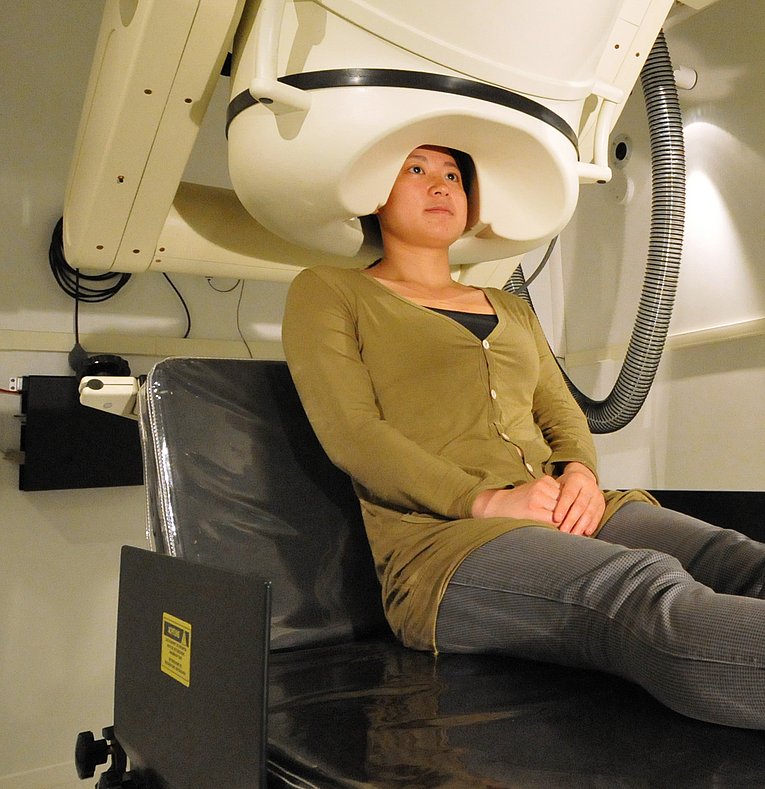
The examination is conducted on the patient who sits or lies down in a relaxed position. The sensitive magnetic field sensors are positioned around the head as closely as possible. The examination requires a preparation time of approximately 30 minutes. The actual examination is usually divided into several parts lasting between 10 and 30 minutes.
Findings
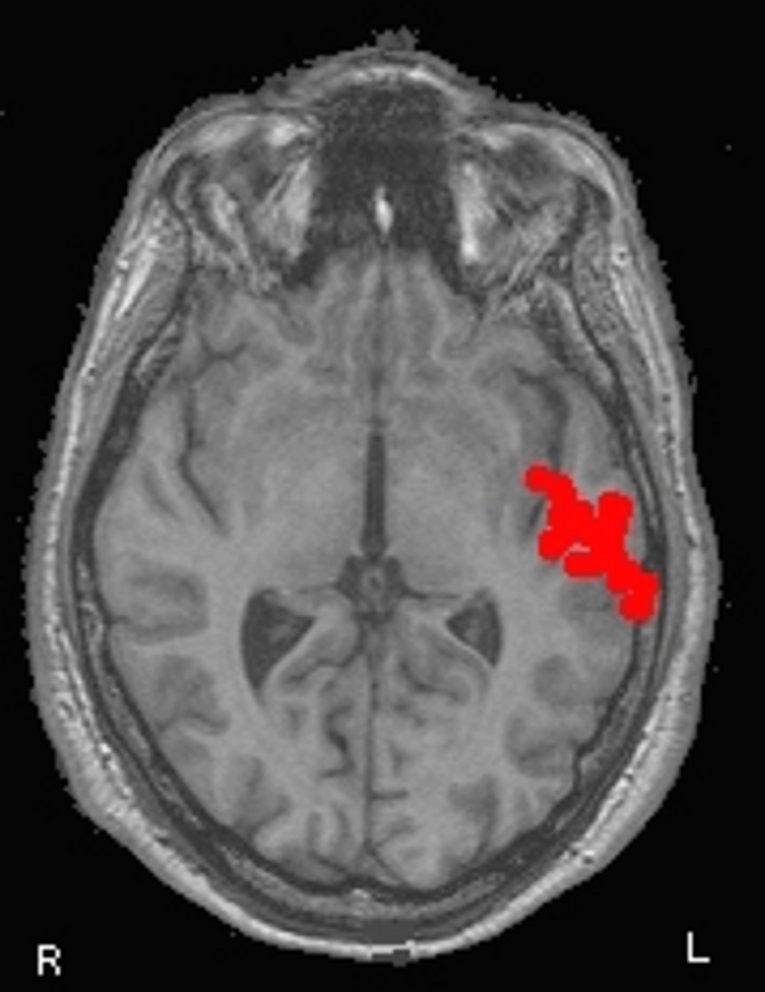
The analysis of the MEG examination usually takes several hours. To be able to visualise the results of the MEG examination in view of a patient's individual brain anatomy, it is also necessary to conduct an imaging procedure. At our Centre, every MEG examination is conducted together with a magnetic resonance imaging (MRI) scan. By visualising the MEG results in the MRI image slices you get a three-dimensional picture of the magnetic activity in the brain. All examination results can be fed into a computer system used for surgery (neuronavigation).
Development
Since its beginnings around 1970, MEG has undergone considerable technical enhancement. In the US, the procedure has been covered by health insurance since 2002. Due to the technical complexity of executing this examination method and evaluating the results, only very few clinics worldwide have MEG systems at their disposal. The Epilepsy Centre got its multichannel MEG system in 1990.
Scientific benefits
The Epilepsy Centre investigates the impact of the combined use of MEG and EEG on the accuracy of pinpointing affected brain areas. The results collected to date show that it is easier to identify the brain areas with over-activity caused by epilepsy by combining the two methods. Also the need for risky invasive measurement methods for which electrodes are attached directly to the brain is significantly reduced, allowing for patient-friendly procedures.




