For the epilepsy treatment of our patients, we collaborate closely with other sections of the Department of Neurosurgery, whose diagnostic procedures we can use if it is required in the individual case. In addition to the outpatient clinics of the Departments of Psychiatry, Ophthalmology and Neuropathology, we work particularly closely with the specialist Departments of Neuroradiology and Nuclear Medicine, where state-of-the-art medical devices are available to carry out examinations which can be carried out in only a few selected medical centres in Germany. In preoperative epilepsy diagnosis, the following imaging techniques are particularly important:
MRI (magnetic resonance imaging)
Due to its high sensitivity and specificity, magnetic resonance imaging (MRI) is the imaging method of choice for epilepsy diagnosis and is essential for preoperative epilepsy diagnosis. It is a patient-friendly, risk-free examination method with only a few contraindications (i.a. pacemakers, magnetizable metal clips and bone implants).
Our Department of Neuroradiology has one of the most modern magnetic resonance imaging devices available, capable of producing images at the highest possible quality. Special T1 and T2-weighted coronal and axial sequences optimised for the purposes of epilepsy diagnosis are used. In order to obtain a reliable image of all regions, in particular in the area of the brain's temporal lobe, the coronal slices are arranged in very thin layers seamlessly and orthogonally to the long axis of the hippocampus. In addition, a three-dimensional volume acquisition is performed. These sequences are followed by inversion recovery sequences for detecting cortical changes in particular.
The objective of this method is to identify even the smallest, discrete epileptogenic lesions by means of magnetic resonance imaging. The most common pathological conditions accompanied by chronic temporal lobe epilepsy are: hippocampal sclerosis, cortical malformations, gliotic changes, low-grade malignant tumours and vascular anomalies. A volumetric analysis of the hippocampi can supplement the qualitative analysis, during which even discrete volume reductions in the structures described may be discovered.
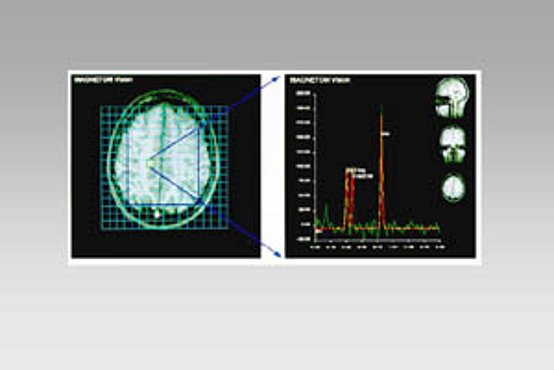
Spectroscopy
Proton MR spectroscopy is another non-invasive magnetic resonance imaging procedure which can detect metabolic changes in the epileptogenic focus area. It measures, among other things, signals from the N-acetylaspartate (NAA), creatine and phosphocreatine (Cr), and choline (Cho). Pathological metabolite changes can be detected in the spectroscopy scan even when the MRI still appears to be normal. This method is relevant in preoperative epilepsy diagnosis. In particular, it helps lateralize temporal lobe epilepsies which are still inconspicuous in the MRI.
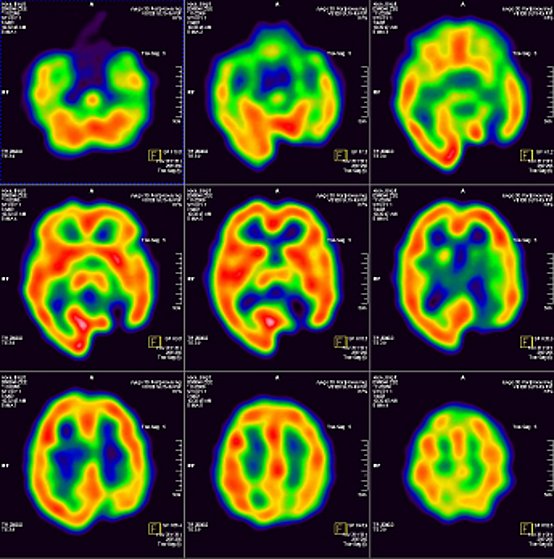
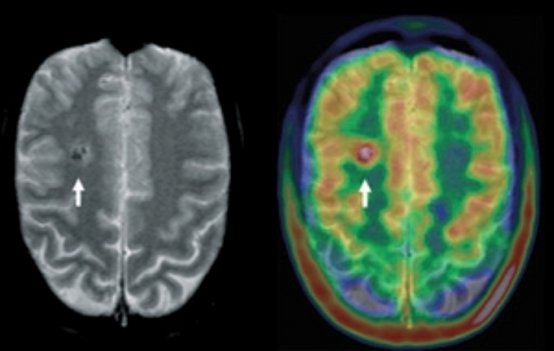
SPECT and PET of the brain
SPECT and PET are two methods from nuclear medicine, using radioactive substances to visualise certain functions of the body. In contrast to computed tomography (CT) and magnetic resonance imaging (MRI), they show functions of the body and not the anatomy of the organ examined. For both methods (SPECT and PET) a radiopharmaceutical, a very slightly radioactive substance, is administered. After a certain waiting time, a special camera takes an image, producing cross-sectional images which visualise certain brain functions like a map.
Radiation exposure is very low. Depending on the examination method, we will give you further instructions to ensure that radiation exposure is as low as possible. The radioactive substances used (isotopes) have a short half-life of between 2 and 13 hours, and the quick decay also ensures low radiation exposure. Side effects related to drug intolerances or allergies are extremely rare.
SPECT
SPECT stands for single photon emission computed tomography.
Most of the time it is used to visualise the blood flow in the brain in seizure-free phases. After a period of rest of approximately 15 minutes, the radiopharmaceutical is administered and then spreads throughout the brain within a short period of time, depending on the blood flow. 30 minutes later, an image is taken using a special camera (a SPECT gamma camera). The process of taking the image is painless and lasts approximately 30 minutes. While the image is taken, the head must not be moved. Analysing the images is complex and takes significant time so patients are advised of the results at a later stage and not immediately following the scan. SPECT can be performed both in the outpatient clinic or during an inpatient stay.
Reduced blood flow often indicates seizure foci. SPECT may identify this regardless of whether there are any changes detected in the CT and MRT scans.
Visualising the blood flow during epileptic seizures is much more time-consuming and requires that the patient stay at the monitoring station. In this case, the radiopharmaceutical is injected as early as possible after the onset of the seizure. The further course of the examination does not differ from an examination in seizure-free phases. In SPECT, the seizure foci are identified due to increased blood flow.
In rare cases, it is also necessary to visualise the benzodiazepine receptors in the brain, which is similar to visualising the blood flow at rest. The waiting period between the injection and taking the image is two hours. It is necessary to disrupt the thyroid function using Irenat®.
PET
PET stands for positron emission tomography. Most of the time it is used to visualise the brain's glucose metabolism. The patient must not eat anything after 8 p.m. on the previous evening and may only drink calorie-free beverages (water, unsweetened tea). After a short period of rest, specially marked glucose is injected which is broken down slowly by the brain in line with the energy metabolism. One hour later, an image is taken with a special camera (PET scanner).
The process of taking the image is painless and lasts approximately 35 minutes. While the image is taken, the head must not be moved. If applicable, anaesthesia may be considered in the case of nervous patients, requiring previous planning. The results are not available directly after the examination. Reduced glucose uptake indicates seizure foci. Compared with SPECT, which examines the brain blood flow, the resolution is twice as high and visualisation of foci between seizures is thus better. However, PET is also much more expensive.




