Medication therapy

The majority of people can become seizure-free by taking suitable antiepileptic medication. Today, there is a wide range of drugs with different active agents which can be used to treat epilepsy. Your physician decides which drugs should be chosen and in what dosage, taking into account the form of epilepsy diagnosed, potential concomitant diseases or interactions with other drugs. Combination therapy involving various different active agents may be required.
To find out which drugs are most effective, the patient should document the course of the disease in a seizure diary as each antiepileptic drug's efficacy must be tested individually in each patient's case.
Approximately 70% of all epilepsy patients can become seizure-free by taking medication. The therapy's continued success is dependent on the regular use of the prescribed medication. Patients must not change the dosage without consulting their physician first. If patients would like to resort to other treatment options because of unpleasant side effects, they should discuss this with their physician.
For a small number of patients, medication therapy is not feasible due to unacceptable side effects or insufficient seizure freedom – these forms of epilepsy are referred to as being drug-resistant. There are further therapy options available for patients with these forms of epilepsy.
Epilepsy surgery

If medication is not enough, surgery can often help to become seizure-free or at least significantly reduce the number of seizures.
In the interdisciplinary conference, neurologists, neuropsychologists, neurosurgeons, neuroradiologists, neuropathologists and medical specialists in nuclear medicine discuss in detail whether epilepsy surgery treatment should be conducted.
In this regard, the Epilepsy Centre collaborates closely with the working group which is conducting research on epilepsy surgery at Universitätsklinikum Erlangen's Department of Neurosurgery.
This interdisciplinary collaboration of several subject areas was the reason that the Epilepsy Centre was established and why the Federal Ministry of Health (BMG) awarded the Centre the highest level of care (level IV) in epileptology. The Epilepsy Centre is one of four centres in Germany with a level IV status.
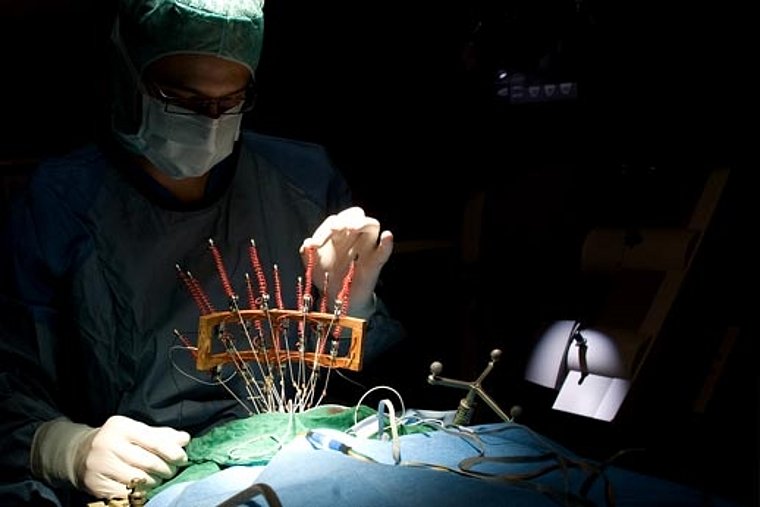
If the interdisciplinary conference opts for surgery, the physicians involved plan and conduct every operation carefully using state-of-the-art technology.
There are several methods of epilepsy surgery. The decision as to which method is used in the individual case is based on the diagnostic findings.
- Surgical resection
- Surgical disconnection
- Vagus nerve stimulation
- Radiotherapy
Surgical resection:
Epileptogenic tissue is removed from the brain with the objective of obtaining seizure freedom.
To be able to treat epilepsy with surgical resection, it is important that the epileptic focus can be clearly isolated.
There must be only one focus (unifocal) which must not be located in eloquent brain areas (e.g. areas responsible for speech or motor skills) and the focus must be accessible to the neurosurgeon. In order to achieve the best possible therapeutic effect while removing as little tissue as possible, a technique called tailored resection was developed. For this surgical technique, the extent of tissue to be removed is determined using EEG recording for which electrodes are placed on the exposed surface of the brain (electrocorticography, ECoG). Neuronavigation systems, including MEG and intraoperative MRI scanners, are available to plan function-preserving epilepsy surgery.
Surgical disconnection:
Disconnection is used where resection is not possible. By severing specific nerve fibres the distribution of seizure impulses in the brain is interrupted.
In multiple subpial transection (MST), nerve fibres are cut through directly beneath the cerebral membrane. This option is used, for instance, in cases where epileptic foci are located in eloquent brain areas.
In corpus callosotomy (cutting the corpus callosum), nerve fibres are severed further beneath the brain surface. In most cases, it is not possible to achieve complete seizure-freedom. However, for patients suffering from severe drop seizures, it does represent a considerable relief.
Further information
Radiotherapy
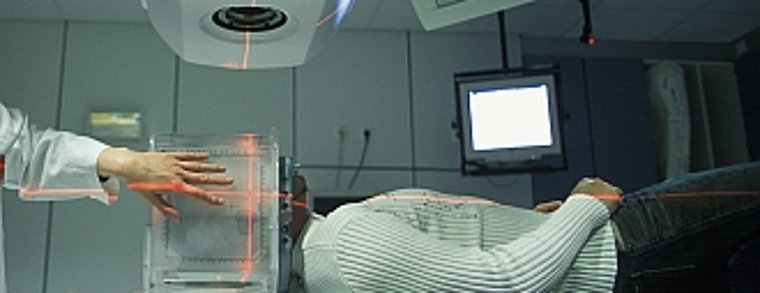
In individual cases, we offer radiotherapy (irradiation).
The epileptogenic focus is treated with targeted radiation (focal stereotactic fractionated low-dose radiotherapy).
This new method can be used for patients in whose case surgery was not effective and it can be expected that radiation will achieve a sufficiently good result.
Further Information
Vagus nerve stimulation

The stimulation of a particular nerve which can also help suppress seizures is another alternative option if surgery is not possible.
The efficacy of vagus nerve stimulation is based on the electrical stimulation of the vagus nerve and is intended to suppress epileptic seizures.
The stimulator itself is a device which can be compared with a pacemaker. It is implanted below the collar bone beneath the skin and is connected with the vagus nerve via an electrode in the neck area.
Quite often, vagus nerve stimulation helps patients in whose case surgery is not an option, such as patients who have several epileptic foci or a focus in an area which is not accessible to a neurosurgeon.
These procedures are likewise performed in the neurosurgery unit of the Department of Neurosurgery.





